
Healing Hemorrhoids: How Self-care and Pelvic PT Can Help
Clinically reviewed by Liz Miracle, PT, MSPT, WCS.
“Don’t look at my butt, I have so many hemorrhoids!”
If pelvic PTs had a nickel for every time we heard this from patients… we’d all be retired on a remote island somewhere.
Hemorrhoids are incredibly common. 4–8% of adults in the U.S. self-report having hemorrhoids, but the real number is much higher: routine colonoscopies identify hemorrhoids in almost 40% (!!) of middle-aged adults.
Despite how common they are, many people don’t discuss hemorrhoids with their healthcare providers. Some people may not realize they have hemorrhoids because they don’t have pain or other symptoms. Others may feel too embarrassed to bring up the topic.
At Origin, though, hemorrhoids aren’t taboo: we recognize that they’re very treatable, and talking about these problems helps more people get care sooner.
Let’s dig in and discuss the causes of hemorrhoids and the treatment options—including pelvic physical therapy—that address them.
What Do Hemorrhoids Feel Like?
Hemorrhoids are swollen veins in the anus. They can develop in the inner or outer portion of the anal canal (or both), and their location affects the symptoms they cause.
What are external hemorrhoids?
These hemorrhoids develop under the skin in the outer third of the anus. They can be painful, especially if a clot (thrombosis) forms inside them. External hemorrhoids can cause swelling, itching, and visible lumps near the anal opening.
What are internal hemorrhoids?
These hemorrhoids form in the inner two-thirds of the anal canal. The nerves in this portion of the anus work differently from those in the outer third: they don’t cause the same type of pain . As a result, internal hemorrhoids can be painless.
Even if they don’t hurt, though, internal hemorrhoids can still cause symptoms. They may bleed during bowel movements: you’d see bright red blood in the toilet bowl if this happens.
If they descend, or “prolapse” out of the anal canal, they can cause skin irritation, mucus discharge or a feeling of “fullness” in the anus. Some people also experience leakage of stool.
Important: If you’re experiencing anal bleeding or noticing blood in your bowel movements, always talk to a healthcare provider. It’s important to rule out other causes before assuming the bleeding is from hemorrhoids.
What causes hemorrhoids?
The processes that lead to hemorrhoid formation still aren’t perfectly clear to scientists. Currently, the most accepted theory is that the supportive tissues in the anal canal break down, allowing the veins to bulge and move downward.
What causes these tissues to break down in the first place? Several factors can contribute, including:
- Aging (hemorrhoids become more common after age 45)
- Straining* during bowel movements
- Sitting for long periods, especially on the toilet
- Low-fiber diets
- Heavy lifting
- Obesity
- Pregnancy and childbirth
- Chronic bowel problems that cause persistent diarrhea
Some research suggests that your body position during bowel movements may also contribute to hemorrhoid formation. In cultures in which people squat to poop, hemorrhoids are less common.
*Although many people associate straining to poop with constipation, it’s not the only cause. Some people strain for other reasons, such as lifelong habits or abnormal pelvic floor muscle patterns.
Hemorrhoids during pregnancy and postpartum
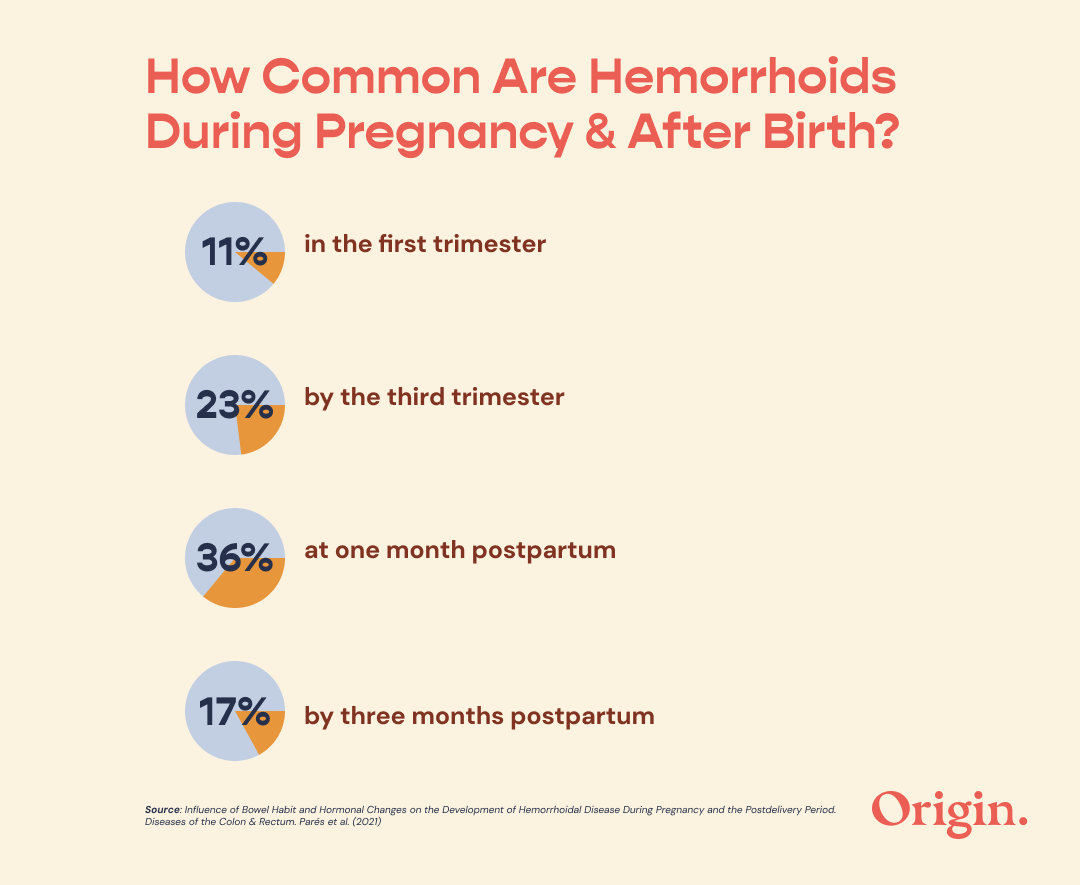
Hemorrhoids are quite common during pregnancy and after birth. A recent study of over 100 pregnant and postpartum people measured the prevalence of hemorrhoids by stage. The results were telling:
- 11% had hemorrhoids in the first trimester
- 23% had hemorrhoids by the third trimester
- At one month postpartum, 36% had hemorrhoids
- By three months postpartum, hemorrhoid prevalence had decreased to 17%
That’s a lot of people living with hemorrhoids!
“As pelvic PTs, we see so many birthing people with hemorrhoids who are embarrassed to discuss them. I promise: your pelvic PT is NOT grossed out by your hemorrhoids. We know they are a common part of the birthing and recovery process, and we’re here to help!” - Liz Miracle, PT, MSPT, WCS
What causes hemorrhoids during and after pregnancy?
Not all birthing people will deal with hemorrhoids. Certain risk factors may increase your likelihood of experiencing them. These include:
- Previous history of hemorrhoids
- Higher BMI
- Constipation
- Recurring diarrhea
- Joint hypermobility
- Having heavier or taller babies
- Birthing multiple children (twins, triplets, etc.)
Here’s the good news: many cases of hemorrhoids improve as your body heals after birth.
However, if symptoms last more than 3 weeks postpartum, there’s a higher chance they’ll become chronic. This is why it’s important to monitor your symptoms for improvement and seek care early if your hemorrhoids aren’t improving on their own.
How long do hemorrhoids last?
As with many medical conditions: it depends.
Many mild hemorrhoids resolve quickly with basic home care. Others may take longer—weeks or sometimes months—to clear up. In some cases, hemorrhoids can become a recurring or chronic issue.
We have more specific data on the trajectory of hemorrhoids in pregnant and postpartum folks. A 2024 study followed over 250 women through pregnancy and the postpartum period. The researchers found that:
- Almost half (45%) of the women experienced full resolution of their hemorrhoid symptoms just a few days after delivery.
- 27% reported that their symptoms resolved in a few weeks.
- 28% said that their symptoms took several months to clear up.
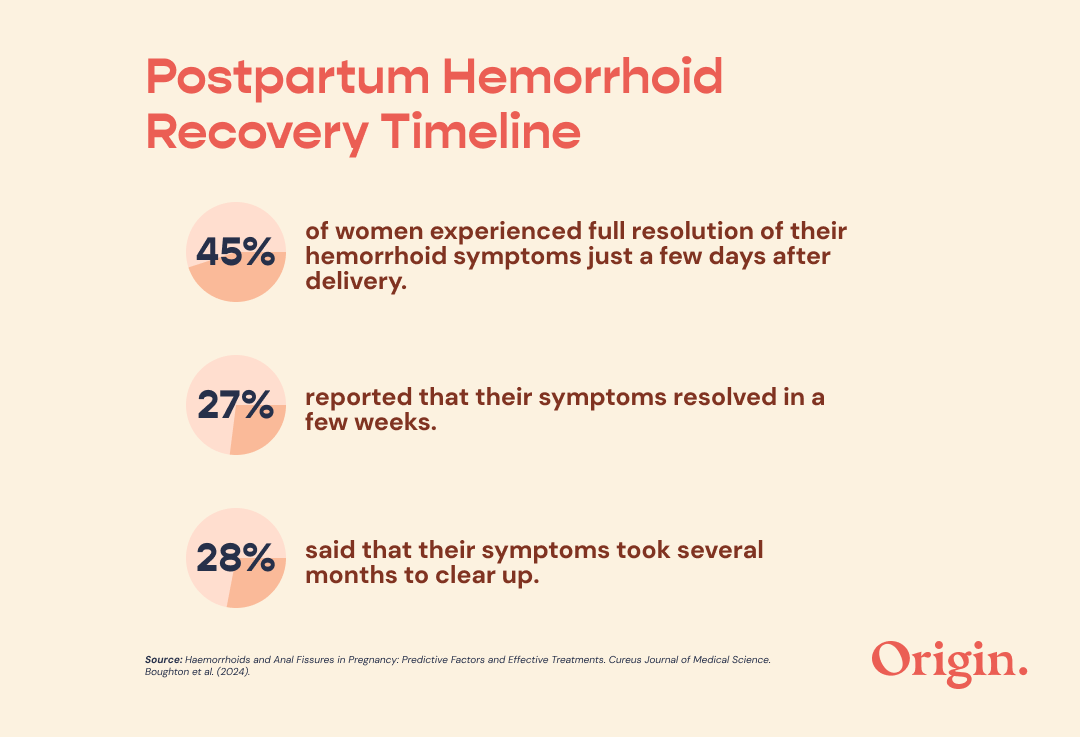
This is great news: almost three-quarters of postpartum people recover from hemorrhoids within a few weeks!
What are my treatment options for hemorrhoids?
Here’s the best news of all: hemorrhoids are generally very treatable. Whether you’re looking for hemorrhoids treatment at home or seeking in-person care, you have options.
Simple habit changes and self-care are first-line strategies for postpartum hemorrhoids treatment. They can also be helpful for people with hemorrhoids from other causes. These strategies can include:
- Take warm, salty sitz baths. Aim for 10 minutes, 3x/day.
- Use glycerin suppositories about 20 minutes before pooping. These dissolve to lubricate the rectum and ease the pooping process.
- Consider adding a bulk-forming fiber supplement such as psyllium husk to your diet.
- To reduce discomfort and bleeding, consider applying witch hazel topically. This herbal remedy is naturally astringent and anti-inflammatory, and it helps constrict blood vessels where it’s applied.
Did you notice that creams like Preparation H don’t appear on this list? That’s because multiple research groups have studied these topicals and found that they aren’t effective for hemorrhoids—so don’t waste your money!
Adjusting your dietary and bathroom habits are additional important shifts, whether you’re focused on hemorrhoids after pregnancy treatment or treating hemorrhoids from other causes.
- Increase your fiber intake by focusing on fiber-rich foods such as fresh fruit, veggies, and whole grains like bran. Sufficient fiber intake can reduce bleeding from hemorrhoids by about half!
- Aim for at least 1.5 liters (about 6 cups) of water intake each day.
- Move your body to move your bowels: even just half an hour of walking can make a difference.
- Listen to your body’s signals: don’t ignore the urge to have a bowel movement.
- Avoid straining or breath-holding during bowel movements.
- Limit time spent on the toilet: if it’s been more than 3 minutes, put down your phone and get off the pot!
Speaking of time on the pot…Western toilets might be additional aggravating factors. Our modern commodes force us to sit upright while pooping, and this body position changes the angle of the rectum.
In contrast, squatting puts your hips into a sharp angle that opens the rectum. This opened angle facilitates bowel movements and can make pooping a quicker, smoother process.
Of course, squatting on a standard toilet is neither comfortable nor safe—but you can solve for this by using a stool to create the same angle at your hips. Check out Origin’s favorite stool options here.
When to see a provider for hemorrhoid treatment
Don’t ignore symptoms that are severe or ongoing, particularly if you’re self-treating hemorrhoids at home. There’s no wrong time to seek help with hemorrhoids, especially if your symptoms are interfering with daily life: the sooner, the better!
Can pelvic floor PT help with hemorrhoids?
In short: you bet!
Many people don’t realize how much pelvic physical therapy can help with hemorrhoids. After all, if you Google “hemorrhoids treatments near me”, you’ll probably get countless results for GI and colorectal specialists before you see a pelvic PT’s website.
Despite its lower public profile, pelvic physical therapy can be a critical tool for people dealing with pooping problems, including those connected to hemorrhoids.
A pelvic PT can help you learn and personalize your approach to the habit changes discussed above. In addition, pelvic PTs are the experts you need to address pelvic floor muscle problems that may influence your hemorrhoids.
Even if you don’t have a pelvic PT near you, you have options! At Origin, we offer virtual physical therapy appointments for all sorts of symptoms, including hemorrhoids treatment at home.
How does pelvic PT help hemorrhoids?
When compared to their peers without hemorrhoids, people who have hemorrhoids often exhibit two patterns that suggest pelvic floor problems:
- At rest, the pressures inside their anal canals are higher, indicating increased tension of the muscles surrounding the anus.
- During bowel movements, their pelvic floor muscles don’t contract and relax in a coordinated fashion. This is called “dyssynergia”, and it can make pooping more difficult.
As you might guess, increased pressure in and around the anus isn’t great for healing hemorrhoids. Fortunately, your pelvic physical therapist can help you address these issues.
In physical therapy for hemorrhoids, you’ll learn how to fully relax and lengthen your pelvic floor muscles to reduce tension at rest. Your pelvic PT can also help you retrain your pelvic floor muscles to improve coordination during toileting.
Pelvic PTs use a variety of techniques to help you achieve these goals, from therapeutic exercises and habit training to hands-on manual treatments and dry needling.
These techniques are highly effective. A clinical trial of pelvic PT for chronic anal fissure—a condition related to hemorrhoids—showed that pelvic PT:
- Reduced resting muscle tone in the anus: basically, the muscles surrounding the anus became less tense and tight.
- Improved coordination of the pelvic floor muscle during bowel movements.
- Decreased the anal pain and other symptoms patients experienced.
I’d call that a win for pelvic health!
You don’t have to suffer with hemorrhoids
As pelvic PTs, we see patients struggling with hemorrhoids and anal symptoms every day. Happily, we get to see how much these patients improve with treatment.
If you’re dealing with hemorrhoids, you’re not alone, and you don’t have to just “live with them”. Conservative care can go a long way, and for many people, pelvic physical therapy may be the missing link.
When you’re ready to address your hemorrhoid symptoms, an Origin provider can support your recovery. Book a visit today to start feeling better tomorrow.
Sources Cited
Admuthe, Namdeo Bhagwan et al. “Natural Products in Hemorrhoid Management: A Comprehensive Literature Review of Traditional Herbal Remedies and Evidence-Based Therapies.” Cureus vol. 17,5 e83397. 3 May. 2025, doi:10.7759/cureus.83397
Boughton, Rebecca S et al. “Haemorrhoids and Anal Fissures in Pregnancy: Predictive Factors and Effective Treatments.” Cureus vol. 16,2 e53773. 7 Feb. 2024, doi:10.7759/cureus.53773
Chen, Yu-Ying et al. “Prevalence, Characteristics, and Treatment of Hemorrhoids During Pregnancy: A Nationwide Population-Based Cohort Study in Taiwan.” Journal of women's health (2002) vol. 32,12 (2023): 1394-1401. doi:10.1089/jwh.2023.0124
Gardner, Ivy H et al. “Benign anorectal disease: hemorrhoids, fissures, and fistulas.” Annals of gastroenterology vol. 33,1 (2020): 9-18. doi:10.20524/aog.2019.0438
Gülören, Gülbala, et al. “Hemorrhoids, anorectal symptoms, and related risk factors in pregnancy and the postpartum period: A follow-up study.” Journal of Women’s & Pelvic Health Physical Therapy, vol. 48, no. 3, July 2024, pp. 184–193, https://doi.org/10.1097/jwh.0000000000000308.
Heitmann, Paul T et al. “Understanding the physiology of human defaecation and disorders of continence and evacuation.” Nature reviews. Gastroenterology & hepatology vol. 18,11 (2021): 751-769. doi:10.1038/s41575-021-00487-5
Kalkdijk, Jenneke et al. “Functional constipation in patients with hemorrhoids: a systematic review and meta-analysis.” European journal of gastroenterology & hepatology vol. 34,8 (2022): 813-822. doi:10.1097/MEG.0000000000002361
Parés, David et al. “Influence of Bowel Habit and Hormonal Changes on the Development of Hemorrhoidal Disease During Pregnancy and the Postdelivery Period: A Prospective Cohort Study.” Diseases of the colon and rectum vol. 64,6 (2021): 724-734. doi:10.1097/DCR.0000000000001822
Poskus, Tomas et al. “Preventing hemorrhoids during pregnancy: a multicenter, randomized clinical trial.” BMC pregnancy and childbirth vol. 22,1 374. 30 Apr. 2022, doi:10.1186/s12884-022-04688-x
Sandler, Robert S, and Anne F Peery. “Rethinking What We Know About Hemorrhoids.” Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association vol. 17,1 (2019): 8-15. doi:10.1016/j.cgh.2018.03.020
Shirah, Bader Hamza et al. “Hemorrhoids during pregnancy: Sitz bath vs. ano-rectal cream: A comparative prospective study of two conservative treatment protocols.” Women and birth : journal of the Australian College of Midwives vol. 31,4 (2018): e272-e277. doi:10.1016/j.wombi.2017.10.003
van Reijn-Baggen, Daniëlle A et al. “Pelvic floor physical therapy in patients with chronic anal fissure: a randomized controlled trial.” Techniques in coloproctology vol. 26,7 (2022): 571-582. doi:10.1007/s10151-022-02618-9




